PATIENT CENTER
Allergy Shot Hours
Patients must make an appointment for allergy shots. Patients can call at 515-410-9400 on the same day to make appointment.
Policy:
We have a 24-hour cancellation policy. Please call at 515-410-9400 24 hours prior to your appointment to reschedule and/or cancel, otherwise a fee will be billed to you that insurance does not cover. If an unforeseen circumstance has prevented you from following our cancellation policy, please contact our clinic to let us know. No-show fees are to ensure patients access to care.
Tardiness:
Please ensure a timely arrival so that each patient can receive their shots at their scheduled time. If you show up later than your scheduled appointment time, you will need to wait for the scheduled patients to receive their injections first. If your appointment is at the end of the working day (i.e., 5:30pm) and you show up late, your appointment will be canceled. 30-minute wait times are required due to the possibility of anaphylaxis.
If you are late 10 minutes or more and do not call/text, our office may cancel your appointment upon your arrival.
If you know you will be late to your shot appointment due to unforeseen circumstances, please call/text at 515-410-9400 our office prior to your visit to verify if we can still see you the same day. Otherwise, you may reschedule without a fee being charged.
WEST DES MOINES CLINIC
Monday 8:15am to 4:15pm
Tuesday 8:15am to 4:15pm
Wednesday 7am to 5:30pm
Thursday 8:15am to 4:15pm
Friday 8:15am to 4:15pm
ANKENY CLINIC
Monday 8:15am to 11:45am and 12:45pm to 4:15pm
Tuesday 8:15am to 11:45am and 12:45pm to 4:15pm
Wednesday 8:15am to 11:45am and 12:45pm to 4:15pm
Thursday 8:15am to 11:45am and 12:45pm to 4:15pm
Friday 8:15am to 11:45am and 12:45pm to 4:15pm
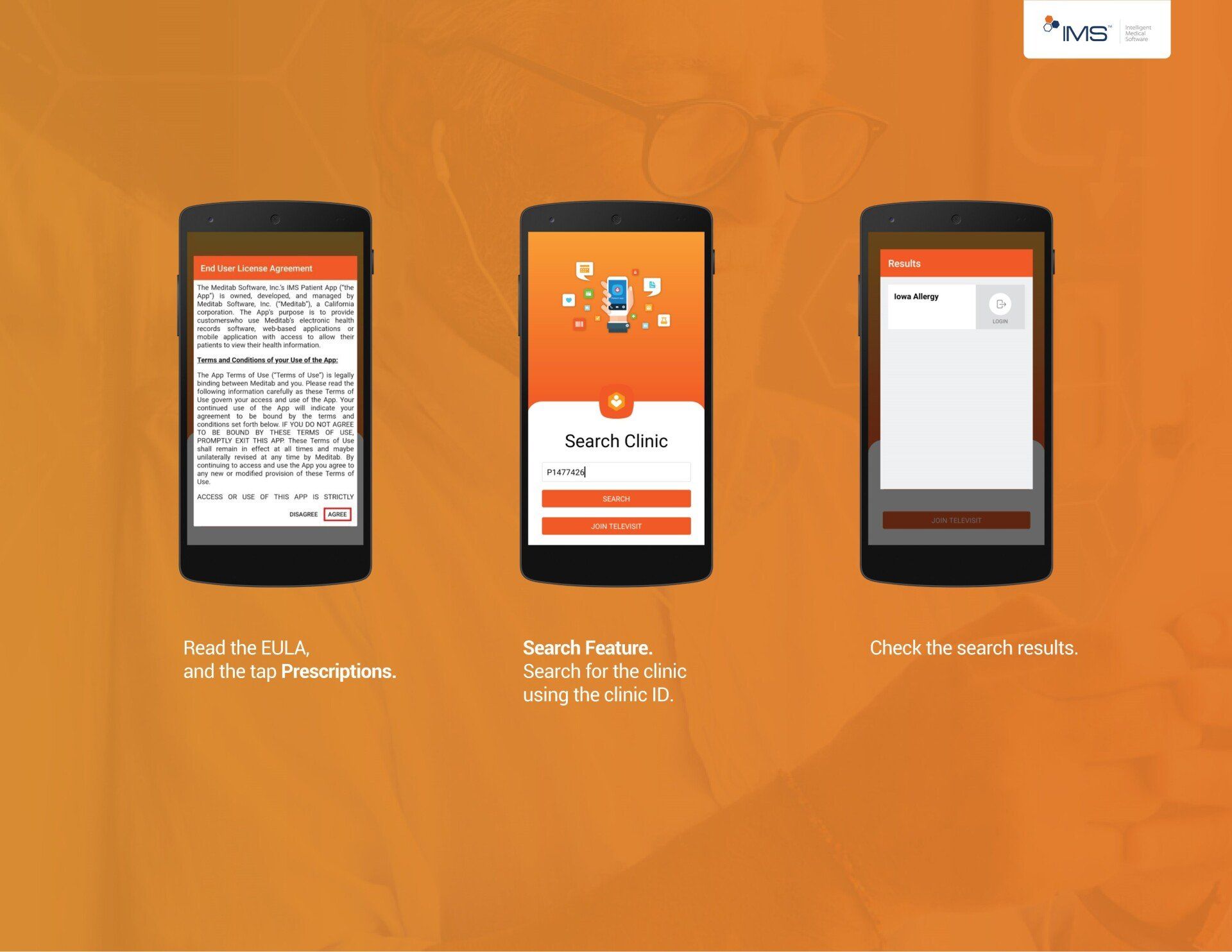
Patient App
We encourage all our allergy shot patients to download and use our patient app to keep track of their appointments and allergy shots.
Inhaler Instructional Videos
This app provides step-by-step instructions, including audio/visual guides, on how to use a variety of inhalers:
https://use-inhalers.com/Home
Televisit
Iowa Allergy provides televisit for all patients. Call/Text us at 515-410-9400 to schedule today.
All testing requires patients to be present in the clinic.
Options for televisits:
- Initial consults (no testing)
- Follow up visit
- Re-evaluation (allergy shot patients only)
- Sick visit
- Medication refills
COVID Response
Iowa Allergy maintains a clean environment in between all patients. Our nurses disinfect each room after patients leave. In addition, Iowa Allergy takes each patient straight to the exam room to wait for the provider to maintain safe social distance measures.
We encourage all our patients to fill out paperwork prior to their visit via our online system. Please click (here) to fill out forms.
Our staff is screened daily for sick symptoms and masks are mandatory in the workplace.
All patients are required to wear a face mask during their entire visit. We ask that patients refrain from handshakes with the providers to reduce the spread of germs.
Medication Coupons
The link below will direct you to a website that is the largest database of manufacturer drug coupons on the internet. They check the links once per week to make sure no coupons have expired. If you have been prescribed a medication, it may be worthwhile to search the site to see if you qualify for any discounts or rebates. If you scroll down on their homepage, you will see coupons arranged by category, including Antihistamine – Hay Fever and Asthma, COPD. You may also select View All Coupons to search an alphabetical list.
https://www.internetdrugcoupons.com/
Additionally, there is a free app available that helps patients easily compare area pharmacies to find the cheapest cost for specific medications. The app also makes patients aware of
medication coupons and gives the availability to use them directly from the user’s mobile device. Below is the link to the iTunes store to learn more about this app.
https://apps.apple.com/us/app/goodrx-prescription-medicine/id485357017
Frequently Asked Questions
Allergy Causes
What is an allergy?
One of the marvels of the human body is that it can defend itself against harmful invaders such as viruses or bacteria. In some people, the body reacts to harmless substances such as dust, mold, or pollen by producing an antibody called immunoglobulin E (IgE). When patients with one of the allergic diseases (such as rhinitis or asthma) are exposed to these substances, the immune system then rallies its defenses, launching a host of complex chemical weapons to attack and destroy the supposed enemy. In the process, some unpleasant and, in extreme cases, life-threatening symptoms may be experience. (acaai.org)
What causes an allergic reaction?
Hundreds or even thousands of ordinary substances can trigger allergic reactions. These are called "allergens." Among the most common are plant pollens, molds, household dust (dust mites), animal dander, industrial chemicals, foods, medicines, and insect stings.
An allergic reaction may occur anywhere in the body, but usually appears in the skin, eyes, lining of the stomach, nose, sinuses, throat, and lungs -- places where special immune system cells are stationed to fight off invaders that are inhaled, swallowed, or come in contact with the skin. (acaai.org)
Allergy Symptoms
The severity and kinds of allergy symptoms depend on a person's genetics, the allergic condition and the type and amount of allergens involved. There are many different types of allergic conditions. An allergic condition is the appearance of allergy signs and symptoms in specific organs or areas of the body. The most common allergy symptoms affect the nose, sinuses, lungs and eyes. However, in some conditions, organs such as the skin, digestive system and blood vessels can be affected as well. Not all allergic reactions happen the same way. Some allergy symptoms occur immediately after exposure to an allergen, while others take hours or days to occur. Scientists think that the biological events leading up to immediate allergic reactions are different from those that result in delayed allergic reactions.
Immediate Allergic Response:
Immediate allergic reactions typically occur within minutes of exposure to an allergen. Allergic reaction time will vary depending on a person's genetics and on the site of the body affected.
Delayed Allergic Response:
Delayed or late-phase allergic reactions generally occur 2 – 6 hours after exposure (and even longer in some people). Signs and symptoms of delayed or late-phase allergic reactions are generally the same as those for immediate allergic reactions.
In the case of allergic asthma, a delayed allergic reaction can cause other problems, such as loss of sleep due to nighttime asthma attacks. There are ways to time allergy and asthma medications to reduce symptoms of the delayed allergic response.
Allergy Tests
What is the best method for allergy testing?
The best first step in the diagnosis of allergies is a through health history and physical examination. If you have allergy symptoms that occur in association with exposure to certain things, that is highly significant. Allergy diagnostic tests, such as skin tests or blood tests, provide similar information and merely confirm what your health history tells the doctor. If your doctor were to rely exclusively on the results of skin or blood tests (without history and physical examination), you could be diagnosed as having an allergic problem that you do not necessarily have.
Skin tests, in most situations, are preferable because:
- The results are available immediately.
- They are less expensive.
- They are more sensitive to subtle allergies.
A blood test is appropriate in certain situations, particularly:
- When you cannot suspend antihistamine therapy which can inhibit skin tests.
- When you have widespread skin disease making skin testing difficult.
- When you are so sensitive to the allergen that the test might be risky.
- When you cannot be skin tested for some other reason. (acaai.org)
How can an allergist help?
An allergist has specialized training and expertise in managing patients with these conditions. They can help you identify causes, triggers and develop a treatment plan for your individual needs. The goal is for you to lead a life that is normal and as symptom-free as possible.
What can I expect during my first allergy visit?
An allergy evaluation has many components. It will include a thorough history of your symptoms, triggers, and environment. A physical exam is performed to aid in making a diagnosis. Many types of diagnostic testing are available as well. This may include allergy skin testing, pulmonary functions, and specialized tests that can be ordered for specific medication, food, or exercise conditions. A treatment plan is designed to address the specific concerns of each patient, with the goal to have each patient understand their disease, as well as its treatment and prevention options.
How long does testing take?
We ask that you allow at least 2 hours for your first appointment, this appointment will include testing and a discussion regarding your medical and environmental history. Please click (here) for more details and videos on testing.
What can I do to prepare for allergy testing?
We ask that each patient stay off antihistamines 5 days prior to their appointment (click here for a list of antihistamines) to be considered for allergy testing. Allergy testing is dependent on each individual patients’ family and personal history.
These are some of the questions to think about to prepare for your visit:
- What symptoms are you experiencing?
- Do your symptoms appear and/or worsen when you are at a particular location, during a given season of the year or at a specific time of day?
- How long have you experienced your symptoms?
- What kind of work do you do? What sort of things are you exposed to at work?
- Are there pets in your home?
- What are your hobbies (i.e., gardening, playing sports)?
- Do any other family members have an allergic condition?
What if I cannot stay off antihistamines?
If you cannot stay off your antihistamines due to the severity of your symptoms, you may not be able to be tested. We do ask for patients to keep their initial consult appointments and our providers will determine the next steps during your visit.
How much does allergy testing cost?
We provide all our patients with pricing transparency sheets. Our billing team checks each individual patients benefits and a breakdown of cost is provided at the time of the visit. If you would like an estimate of services please (click here)
Environmental Allergies Treatment
What options are available for treatment of allergies?
- The most effective approach to treating asthma or allergies is to avoid the factors that trigger the condition in the first place. Even when it is not possible to completely avoid allergens, an allergist can design strategies for reducing exposure and preventing symptoms.
- Medications – Several new and effective medications are available. The goal is to outline what is available and to balance safety and effective plans with what each patient’s needs.
- Immunotherapy (Allergy Injections/Drops) – There are two types of treatments that are offered for our patients:
- Allergy Injections – In this treatment, the patient is injected over the course of time with gradually increasing doses of the substances to which they are allergic. In most cases, the body’s reaction to the substance becomes less pronounced over time.
- Allergy Drops – This is sublingual (under the tongue) and contain allergens in solution that are placed under the tongue. These drops can be safely administered at home daily. This therapy is particularly helpful in young children in hope of preventing the continued worsening of childhood allergies and asthma.
Allergy Shots/ Subcutaneous Immunotherapy (SCIT)
What are allergy shots?
Subcutaneous immunotherapy (SCIT or allergy shots) is the injection of allergens to build tolerance. Allergy shots increase your tolerance to bothersome allergens. By injecting gradually increasing doses of the offending allergen extract, the immune system builds up a tolerance to those allergens. Allergy shots slow down and reduce the production of the IgE antibody. You can think of each shot as adding a brick to the “wall of protection” against things that trigger your allergies.
What do allergy shots treat?
Allergy shots can be used to control symptoms triggered by:
- Seasonal allergies: If you have seasonal allergic asthma or hay fever symptoms, you may be allergic to pollens released by trees, grasses or weeds.
- Indoor allergens: If you have year-round symptoms, you may be allergic to indoor allergens such as dust mites, cockroaches, mold, or dander from pets like cats or dogs.
- Insect stings: Allergic reactions to insect stings can be triggered by bees, wasps, hornets or yellow jackets.
How do allergy shots work?
Allergy shots has two phases: building and maintenance. Building consists of small increases in dosage every 2 to 14 days and continues as patient’s tolerance increases. When building is completed the maintenance phase begins and patients get injections every 14-21 days. Most patients feel some benefit within the first few months of shots but rarely can take up to 12 months to feel some improvement. SCIT generally lasts 3 to 5 years. Reassessments are required the first 3 and 6 months of allergy shots, and annually thereafter.
After 5 years of successful treatment, most patients don't have significant allergy problems even after allergy shots are stopped. A small percentage of people need ongoing shots to keep symptoms under control.
Who should get allergy shots?
You may benefit from allergy shots if you:
- Have symptoms not controlled with allergy medications
- Have side effects from allergy medications
- Want to decrease medication use
- Have allergy triggers that you cannot avoid (e.g., pollen, dust, pets)
- Have severe reactions to stinging insects
- Want to spend more time outdoors
- Want a better long-term solution to your allergy and asthma problems
Allergy shots are very effective in the treatment of allergic asthma. Over time, they can help your breathing and decrease the need for asthma medications. Allergy shots also benefit patients with eczema or atopic dermatitis, when the condition is associated with environmental allergies.
What are the risks of allergy shots?
Most patients do not have major problems with allergy shots. Allergy shots do contain the patient’s allergens so reactions are possible, and can include:
- Local reactions involving redness, swelling, itching or pain at the injection site. These common reactions typically begin within a few hours of the injection and clear up soon after.
- Systemic reactions including anaphylaxis are rare but potentially more serious. You may develop sneezing, nasal congestion or hives. More-severe reactions may include throat swelling, coughing, wheezing or chest tightness. Very rare life-threatening reactions can cause low blood pressure, dizziness, vomiting, and trouble breathing. Anaphylaxis often begins within 30 minutes of the injections but can be delayed by hours.
If you get your shots on a regular schedule without missing doses, you're less likely to have a serious reaction.
Taking antihistamines before getting your allergy shots can reduce the risk of a reaction.
The possibility of a severe reaction is scary — but you won't be on your own. You'll be observed in the doctor's office for 30 minutes after each appointment, when the most serious reactions usually occur. If you have a severe reaction after you leave, administer epinephrine as prescribed and call our office, or call 911, or go to the nearest emergency room.
How do I start allergy shots?
In order to start allergy shots you must have a consultation and testing to figure out your allergies. Please call/text our office at 515-410-9400 to schedule an appointment or click
(here)
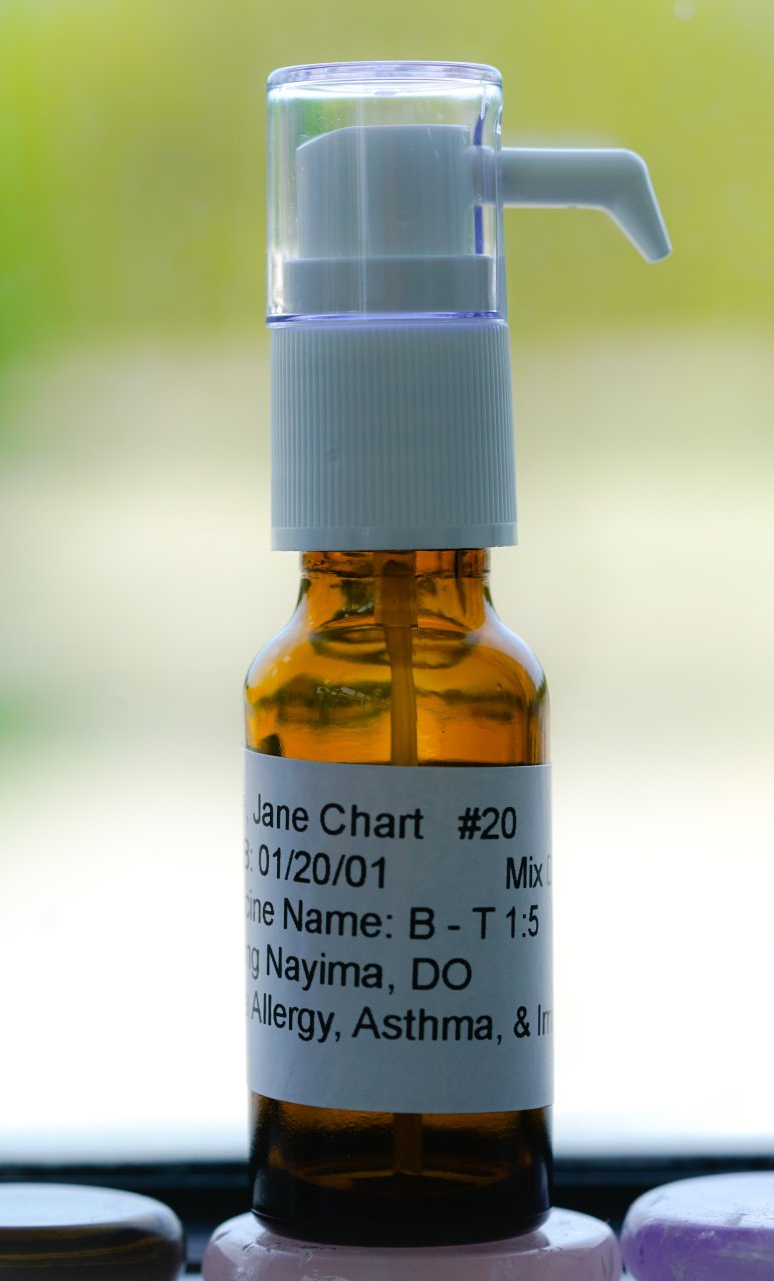
Allergy Drops/ Sublingual Immunotherapy (SLIT)
What are allergy drops?
Sublingual immunotherapy (SLIT or allergy drops) is using liquid allergens under the tongue to build tolerance. Just like allergy shots, allergy drops are customized to the patient with their individual allergies.
What allergies can be treated with allergy drops?
- Seasonal allergies. If you have seasonal allergic asthma or hay fever symptoms, you may be allergic to pollens released by trees, grasses or weeds.
- Indoor allergens. If you have year-round symptoms, you may be allergic to indoor allergens such as dust mites, cockroaches, mold, or dander from pets like cats or dogs.
What are the advantages of allergy drops?
In addition to being a practical option for people of all ages and conditions, there are more advantages:
- Lower cost, fewer clinic visits. Compared to shots and many medications, allergy drops typically cost less over time. Most patients receiving allergy drops need only a few clinic visits the first year, and then once every 6-12 months thereafter until visits are no longer needed. That can also mean a lot less time away from work or school.
- More convenient. You can take allergy drops every day at home or when traveling, making it much easier to stay with your treatment.
- No needles
- Less medication. Our patients report, and research confirms, that they typically need less medication to control symptoms after beginning allergy drops.
Are allergy drops safe?
Allergy drops are not FDA approved in the U.S. but is approved in Europe and has been used for many years with great efficacy and safety. Some studies suggest that SLIT may be slightly less effective than allergy shots, but this has not been definitively proven.
Will my insurance cover allergy drops?
Because allergy drops are an off-label use of FDA-approved antigens, they are not typically covered by insurance. Check with your carrier first. Allergy drops do qualify for Health Savings Account or Flex Spending reimbursement. Even without insurance coverage, most patients find treatment affordable and comparable to other medication or visit co-pays. Most patients agree that the temporary investment in allergy drops is well worth the lasting results and improvement in their quality of life.
How long will I need to do allergy drops for?
SLIT has 2 phases: building & maintenance. Building consists of increases in dosage every day and lasts about 7 days depending on the patient’s tolerance. When building is completed, the maintenance phase begins, and patients continue the same amount of drops daily at home. Maintenance lasts 3 to 5 years.
If the FDA doesn’t approve allergy drops, are they safe to use?
It’s important to understand that the antigens used in allergy drops are the same FDA-approved antigens used in allergy shots. They’re also prepared in the same way as allergy shots. The difference is the route of delivery — a dispenser that delivers a precise drop of antigen under the tongue versus a syringe injecting antigen into tissue. The FDA approves products, not therapies, so it’s unlikely that it will ever “approve” custom, multi-antigen sublingual immunotherapy.
What are the risks of allergy drops?
Common local reactions can occur including itching/redness/swelling of the tongue/throat/mouth. These reactions usually occur within 24 hours and can be treated with oral antihistamines. Abdominal pain, nausea, reflux, diarrhea, and trouble swallowing can rarely occur. Serious reactions include anaphylactic reactions. The first dose of drops is administered in the office under medical supervision because of the potential risk. Subsequent doses are done at home. Allergy drops have been used for many years around the world and there has not been any reported deaths.
How do I start allergy drops?
In order to start allergy drops you must have a consultation and testing to figure out your allergies. Please call/text our office at 515-410-9400 to schedule an appointment or click (here)
Food Allergies
What is a food allergy?
A true food allergy involves the abnormal response of the body’s immune mechanisms to specific foods or food ingredients. A wide variety of symptoms can occur with a food allergy and usually fall into these categories:
- Gastrointestinal: abdominal pain, nausea, vomiting, diarrhea, trouble swallowing
- Skin: itching, hives, swelling, rash
- Upper and lower respiratory: asthma, cough, nasal symptoms, watery/itchy eyes, throat swelling, hoarseness, shortness of breath, wheezing
What foods cause allergic reactions?
Foods that commonly cause allergy in infants and children are egg, milk, peanuts, soy, wheat, and fish. Foods that commonly cause allergy in adults are shellfish, peanuts, nuts, fish, and soy. However, food allergy may develop to any food that is included in the diet and may develop at any time in life.
What are the differences between a food intolerance and food allergy?
Food allergy is sometimes confused with food intolerance. Food allergies involve your immune system, are predictable, and can be life-threatening. An intolerance is when your body has an abnormal response to a food or chemical is irritating to the body but does not involve the immune system. Intolerances can be unpredictable and can cause symptoms but is generally much milder than true allergy.
What are symptoms of a food reaction?
An allergic reaction to food can have many different symptoms, and a single person can experience different symptoms from one reaction to the next. Many reactions start with skin symptoms, like hives or a rash, but some do not. More serious symptoms like a drop in blood pressure and trouble breathing can be life-threatening. Talk to your allergist and work with them to figure out a plan for emergencies.
What is Anaphylaxis?
Anaphylaxis is a serious, severe allergic reaction that comes on quickly and may cause death. Early use of an epinephrine auto-injector is the primary treatment for anaphylaxis.
Anaphylaxis often begins within minutes after a person eats a problem food. Less commonly, symptoms may begin hours later. Up to 20 percent of patients have a second wave of symptoms hours or even days after their initial symptoms have subsided. This is called biphasic anaphylaxis.
Anaphylaxis is highly likely to be occurring when any one of the following happens within minutes to hours after ingestion of the food allergen:
- Difficulty breathing
- Throat tightness
- Change in voice
- Coughing
- Runny nose/congestion/sneezing
- Itchy/red/watery eyes
- Reduced blood pressure (e.g., pale, weak pulse, confusion, loss of consciousness)
- Racing heart
- Sense of impending doom
- Hives, itching, or swelling of any body part
- Gastrointestinal symptoms (e.g., vomiting, diarrhea, cramping)
How are food allergies treated?
Once a food allergy is suspected, your provider will determine if you are a candidate for a food challenge to confirm or reject the allergy or desensitization to build tolerance to the food. There are several factors involved with this decision-making process that may include skin testing, blood tests, and patient history.
There are 3 options for food allergy:
- Avoidance of the food and carrying an epinephrine auto-injector for accidental exposures.
- Food challenge is a process by which a small amount of food is given by mouth in increasing doses over the period of up to several hours under the supervision of a provider. This is done when there is a good chance that you may not be allergic to the food. Please click (here) for more information.
- Desensitization (oral immunotherapy) refers to feeding an allergic individual an increasing amount of an allergen with the goal of increasing the threshold that triggers a reaction. For example, peanut-allergic patients can be given very small amounts of peanut protein in increasing amounts in the allergist’s office. The goal of therapy is to raise the threshold that may trigger a reaction and provide the allergic individual protection against accidental ingestion of the allergen.
Desensitization - Oral Immunotherapy (OIT)
OIT is a process by which a food-allergic patient is given very small amounts of the food by mouth in increasing doses every day over a long period of time in order to achieve tolerance to that food. Tolerance is defined as no symptoms or only having mild symptoms if the food is ingested. OIT and is still investigational as the studies examining its safety and effectiveness have only been around for a few years. OIT is NOT FDA-approved as a treatment for food allergy. However, published evidence has been supportive.
Why do OIT?
The goal of OIT is to prevent the person who is allergic from having an allergic reaction if they are accidentally exposed to their allergen or possibly if they eat a larger amount of the allergen. Some patients can continue to tolerate the allergen even after stopping OIT while others must continue OIT in order to stay desensitized. Patients undergoing OIT will need to continue to avoid their allergen and always carry their epinephrine auto-injectors with them.
How effective is OIT?
Depends on the food. For example, in clinical trials for peanut allergy about 80% of patients were able to be desensitized, meaning they were able to tolerate more peanut following OIT than they did prior to OIT.
What are the risks/side effects of OIT?
There are expected allergic reactions during OIT, the most severe tend to be on the initial escalation day and the build-up phase but can happen at any time even after being on maintenance for years. Reactions range from mild (runny nose, itchy eyes/mouth, hives around the lips, nasal congestion, etc.) to severe (shortness of breath, throat swelling, diarrhea, stomach pain, loss of consciousness, generalized hives, anaphylaxis) and death (theoretically) although this has not been reported for OIT that we are aware of.
There have also been a few reports of patients who are receiving OIT developing eosinophilic esophagitis, a condition characterized by inflammation of the esophagus and difficulty swallowing. Overall, about 10-20% of patients drop out from OIT, usually due to side effects like abdominal discomfort.
What does the schedule look like for OIT?
- Initial escalation day: this day takes about 6-7 hours and extremely small amounts of food protein is introduced by mouth (in a safe food that patient brings such as applesauce or yogurt) in increasing doses every 30 minutes. We find a dose at which the patient has very little or no symptoms and we use this as the home dose. Patient is to purchase an acceptable scale to measure doses at home, pick up medications to treat reactions, and have a journal to record daily doses, reactions, etc. All questions and details are addressed at this time including self-measurement of doses.
- Build-up phase: after initial escalation day, patient will continue this dose daily at home while eliminating all other ingestion of the food in the diet unless discussed with a provider. S/he will come back to the office every 1-4 weeks to do a dosage increase until we are able to reach a maintenance dose. If the patient is less than 3 years old, the maintenance dose will be lower.
- Maintenance phase: Once the maintenance dose is tolerated, the patient continues to ingest that dose of food daily at home in the maintenance phase and comes back to the office every 4-6 months to do a food challenge to see if s/he is able to tolerate a higher dose of that food. Goal of the maintenance phase is to continue the highest tolerated dose daily for the longest possible amount of time. We aim for at least 3 years but may recommend a longer duration depending on the clinical scenario. Some patients, after being on OIT for a few years, exhibit signs that they will tolerate that food indefinitely after stopping OIT. Others will need to continue maintenance phase to maintain tolerance. Evidence points to children under 3 years old benefiting more from OIT and having a higher chance of having tolerance after stopping OIT than older patients.
What is my responsibility as a patient and/or parent?
The desensitization process is laborious and requires vigilance, honesty, and determination from the patient and family involved. It can be a daunting process, but many believe the result is worth it.